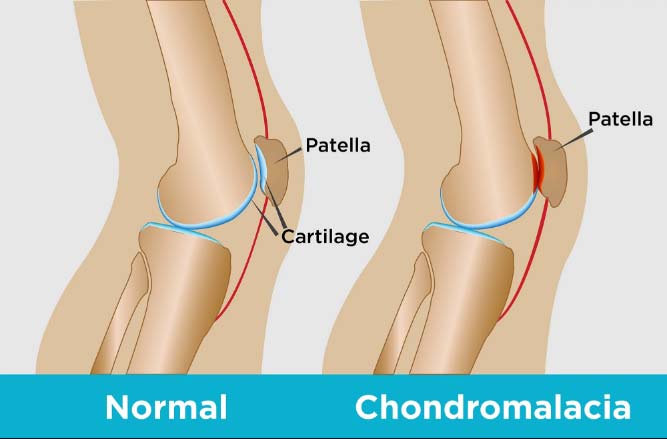
What Is Chondromalacia?
Chondromalacia patellae, also known as "runner's knee," is a condition where the articular cartilage on the underside of the patella or kneecap deteriorates and softens. This condition is common among young, athletic individuals, but may also occur in older adults who have osteoarthritis of the knee.
Causes, Signs And Symptoms
Symptoms of Chondromalacia will typically present as pain in the knee region, known as patellofemoral pain. Most common symptoms of this condition are:
- Pain behind kneecap (patellofemoral syndrome pain or kneecap pain)
- Grinding or cracking when bending/extending the knee (kneecap popping)
- Kneecap pain when walking or standing for long periods
- Warmth, tenderness, swelling. This can also be associated with patellar bursitis which often accompanies chondromalacia
Knee cap pain or patellofemoral syndrome pain typical of Chondromalacia are caused by various musculoskeletal imbalances including the following:
- Poor knee alignment due to a congenital condition
- Weak hamstrings and quadriceps (the muscles in the back and front of your thighs, respectively)
- Muscle imbalance between the adductors and abductors (the muscles on the outside and inside of your thighs)
- Repeated stress to your knee joints, such as from running, skiing, or jumping
- A direct blow or trauma to your kneecap

Chondromalacia can affect the young and old. Here are the most common risk factors:
- Age. Adolescents experiencing growth spurts can cause muscles and bone to develop rapidly creating short-term imbalances.
- Sex. Females are at higher risk as they typically possess less muscle mass than males causing abnormal knee positioning.
- Flat feet. More stress is placed on the knee due to flat feet relative to higher arches.
- Activity level. Frequent, repetitive, high impact activities increase the risk for knee problems.
- Arthritis. Chondromalacia can be a symptom of osteoarthritis where inflammation alters the function of the knee.
Our specialists base their diagnosis of Chondromalacia (Patellofemoral Syndrome) using a multipronged approach:
- Medical History: Our doctors will ask you about the nature of your knee pain (e.g., when and under what conditions you experience knee pain). They will ask about prior surgeries, accidents, and trauma to the knee.
- Physical Exam: The doctor will assess your knee function by testing the range of motion, pain when kneeing, listen for any cracking or popping noises (crepitus), and perform a patellar grind or Clark's test to test for chondromalacia.
- Imaging with X-Rays or MRI: X-rays can diagnose osteoarthritis of the knee which can co-occur with chondromalacia but are not sufficient to diagnose chondromalacia. Blood tests can rule out other forms of arthritis. More advanced imaging like magnetic resonance imaging (MRIs) will be required to determine the extent of damage to the knee.
- Arthroscopy: A tiny, flexible camera can be inserted into the knee to determine the condition of the cartilage.

Treatment Options
The StemX clinic offers a range of regenerative medicine advanced therapy treatments to treat orthopedic injuries.

The StemX Approach
StemX is California's leading provider of holistic and regenerative medicine services. Our experts don't just offer popular treatments, but customized medical solutions based on individual needs.
Located in Solana Beach, California, the StemX clinic is composed of a team of expert doctors with years of experience administering regenerative medicine treatments for joint disease. Our team has:



How To Get Started
Treatment Procedure
While each treatment may be customized, you can expect your experience to be similar to the following:


All procedures are conducted in our Solana Beach, California clinic. 124 Lomas Santa Fe Dr #206, Solana Beach, CA 92075.
Frequently Asked Questions
Mild to moderate chondromalacia can be treated and reversed. Advanced regenerative orthopedic medicine can stimulate the body to repair the weakened cartilage and treat the swollen kneecap.
Chondromalacia (syndrome patellofemoral) and the associated patella tendon pain and pain in kneecap can be treated with regenerative medicine treatments that offer a natural method to stimulate healing by reducing swelling and pain.
Chondromalacia is rarely a severe condition. However, athletes, being overweight, and having experienced trauma to the knee can worsen pain under the kneecap to a point where typical over the counter therapies are no longer useful.
Healing time is variable depending on the severity of the condition, the patient's adherence to therapy (stretching knee cap etc.), and activity levels. Regenerative medicine approaches can reduce the healing time significantly..
Cortisone injections can be helpful for pain management but may adversely affect cartilage health therefore the frequency of use is very limited..
Treatment depends on the needs of the patient. StemX specialists offer customized regenerative medicine treatments together with physical therapy and behavioral modification (activity levels and losing weight) for best results.
Depending on the treatment you and your provider choose, one can see improvement in as little as 3 weeks with maximum effects anywhere from 6-9 months later as the body is stimulated to heal.
No treatment is permanent if the cause of chondromalacia is not also addressed. However, regenerative medicine approaches have been shown reduce pain and increase mobility much longer than cortisone shots.
70% of patients are good candidates for regenerative medicine treatments. Surgery may be the only option for the most severe cases. Allergies, medication concerns, or implants that pose an infection risk may disqualify a patient from treatment.
Regenerative medicine treatments are not painful. They involve simple injections into area around the affect joint which causes minimal discomfort.



